Duchene muscular dystrophy (DMD) is a genetic condition which affects the muscles, causing muscle weakness. It is a serious condition which starts in early childhood. The muscle weakness is not noticeable at birth, even though the child is born with the gene which causes it. The weakness develops gradually, usually noticeable by the age of three. Symptoms are mild at first, but become more severe as the child gets older. Duchene muscular dystrophy, the most common type, is one of more than 20 muscular dystrophies.
The incidence of DMD globally is every 1/3500 male births. All types of muscular dystrophy are caused by faults in genes (the units of inheritance that parents pass on to their children) which result in progressive muscle weakness due to muscle cells breaking down and gradually becoming lost. The Duchene type affects only boys (with extremely rare exceptions) and a problem in this gene is known to result in a defect in a single important protein in muscle fibers called dystrophin.
The symptoms usually start around age 1-3 years, and may include:
Difficulty in walking, running, jumping and climbing stairs. Walking may look different with a 'waddling' type of walk. The boy may be late in starting to walk (although many children without DMD also walk late).
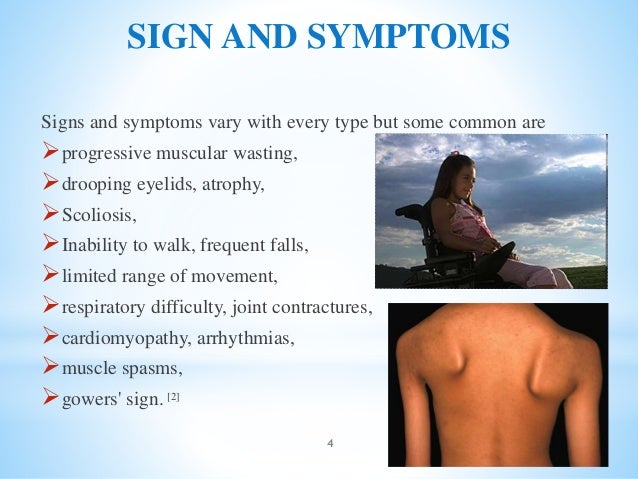
When you pick the child up, you may feel as if he 'slips through your hands', due to looseness of the muscles around the shoulder.
Toe-walking, Frequent falls
The calf muscles may look bulky, although they are not strong.
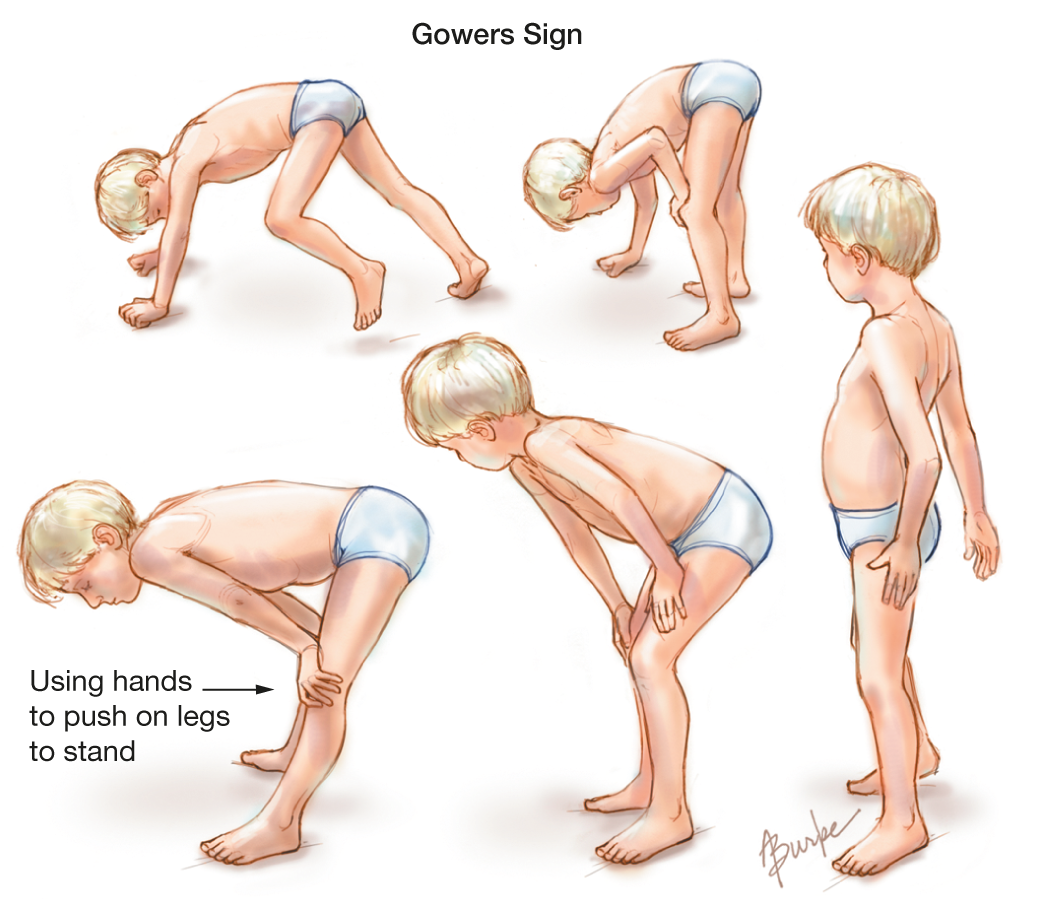
As he gets older, the child may use his hands to help him get up, looking as if he is 'climbing up his legs'. This is called 'Gower's sign'.
PHYSIOTHERAPY MANAGEMENT:

Physiotherapists can help slow the degression of range of motion, muscle strength, daily function, work to improve gait pattern and posture/alignment . Physiotherapy can also address the pain that the patient may be experiencing. As the patient's walking and standing abilities decline the physiotherapist may choose to implement a standing program
Physiotherapists do stretching program with combination of passive range of motion, active range of motion, and active assisted range of motion. Regular stretching of the ankle, knee, and hip is necessary throughout the course of a patient's life. Physiotherapists will teach you, how to stretch these muscles himself.
Role of Physiotherapy in Muscular Dystrophy
The main goal of physiotherapy in patients with MD is to maintain the available function in their limbs and attain maximum possible improvement in the associated disabilities. This would help the patient attain a socially functional status so that he/she can function in the surroundings, of their own accord, bringing about a sense of independence in the patients.
The therapeutic practices involved and their importance in the life of an MD patient are as follows:
- Electrotherapy: A patient with MD often complains of musculoskeletal pains at various sites. Electrotherapeutic modalities like paraffin wax bath over fractured limb, TENS, IFT, Ultrasonic therapy for tender points and Contrast Bath can be done to relieve such pains.
- Passive movement: Passive movements are a technique that involves movement of limbs by the physiotherapist, in all ranges, in a manner so as to maintain joint and muscle integrity. Long term immobilization in patients due to weakness of the muscles can render the muscle fibrotic and the joint may become stiff. To avoid the development of these co morbidities one need to maintain the integrity of structures by passive movements.
- Active assisted movements: The MD patient has limited muscle power. Therefore, with maximum effort, they can attain only a limited range by active contraction of their muscle. To maintain this power, maximum amount activity upto the fatigue threshold should be encouraged in these patients. While the patient maintains muscle force, the physiotherapist should assist the completion of this movement in the normal biomechanical pattern. This will maintain the joint proprioception i.e. the sense of joint position in space.
- Stretching manoeuvres: Often again due to immobility and poor power of muscles, the muscles shorten in length. The joints adapt a gravity assisted position and internal muscular forces cannot work against the external gravitational force. As a result of this joint contractures develop. To open up these joints and retain the normal muscle length, stretching is done on the joints. A sustained long duration stretch with crepe bandages or taping can be given initially and this can be toned down a bit in later stages to short duration stretches with greater repetitions given manually.
- Joint mobilization: Due to imbalance of muscular forces, the joints often get displaced from their normal anatomical position. To guide them back so that proper weight bearing can be done on the joints without causing any harm to the associated structures, the physiotherapist passively mobilizes the bones of each joint to bring them in place.
- Balance and Gait training: Muscular imbalances are so profound in MD that sitting and standing balance are greatly affected in the patients. So with gradual progression from kneeling to quadruped to high sitting to standing position, balance training should be given. As the balance improves the patient will be able to function better by himself/herself. With gradual degradation of power in lower extremities, the locomotion or gait is affected. So gait training involving proper training in parallel bars progressing from supported to unsupported walking should be done under the supervision of the physiotherapist.
- Hydrotherapy: Hydrotherapy or aquatic exercises are an innate part of physiotherapy rehabilitation protocol for MD. Activities are performed in water at a warmer temperature than body. This helps in the following manner:
- Buoyancy of water protects and braces the weak joints.
- In water a person can feel very little of his/her own weight so this makes activities of partial weight bearing possible.
- Adding floatation devices can assist the movements while adding high pressure water jet can help in performing mild resistance training in better muscle groups.
- Warmer water helps in maintaining good thermo-stasis in the body and keeps the active muscle warm and hence at ease.
- Cardiac Pacing and Breathing Exercises: As the muscles of heart and respiratory system weaken, greater chest and cardiac congestion is seen in the patients with MD. To avoid the deleterious effects of an insufficient cardiopulmonary system, one needs to keep in mind a few points.
- Clear airway should be maintained by passive chest manipulations given by the physiotherapist.
- The patient should be taught huffing and coughing to aid him in spitting out the chest secretions.
- Deep breathing exercises should be taught to condition the general cardiorespiratory performance and endurance.

Thank you because you have been willing to share information with us. we will always appreciate all you have done here because I know you are very concerned with our. Physiotherapy in Mississauga
ReplyDelete