Introduction:
The aim of positioning the patient is to try to promote optimal recovery by modulating muscle tone, providing appropriate sensory information, increasing spatial awareness and prevention of complications such as pressure sores, contracture, pain, respiratory problems and assist safer eating.
Correct positioning can help to reduce the risk of;
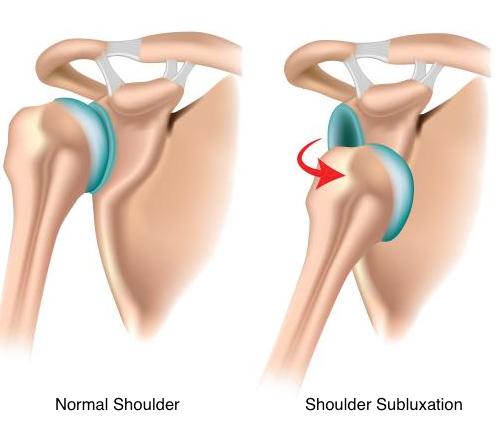
AspirationContracture Pressure AreasShoulder Pain Swelling of the Extremities
Aims of positioning:
Normalise Tone or Decrease Abnormal influence on the Body
Maintain Skeletal Alignment
Prevent, Accommodate or Correct Skeletal Deformity
Provide Stable Base of Support
Promote Increased Tolerance of Desired Position
Increased Stimulation to Affected Side
Increased Spatial Awareness
Promote Patient Comfort
Facilitate Normal Movement Patterns
Control Abnormal Movement Patterns
Manage Pressure
Decrease Fatigue
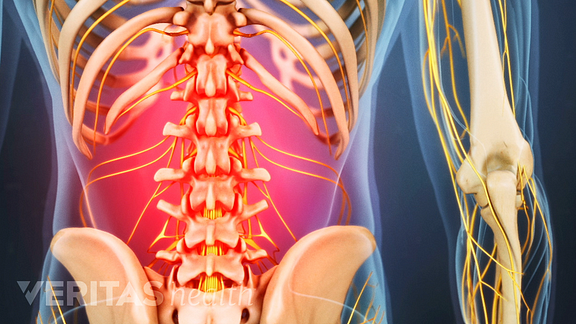
Enhance Autonomic Nervous System Function (Cardiac, Digestive and Respiratory Runction)
Facilitate Maximum Function
Improved Ability to Interact with the Environment
Types of positioning:
1. Sitting in a Chair or Sitting in a Wheelchair:
It is vital that as soon as the person is capable of sitting out that they are facilitated to do so. Sitting out is essential to build up tolerance; provide maximum stimulation; give a sense of normality.
Head over PelvisHips at 90 degreesKnees at 90 degreesSlight extension of lumber regionFeet in neutral position and supportedWeight evenly distributed between both buttocksArm should be protracted forward and supported
2. Side lying on the unaffected side:
The stroke arm should be well forward, keeping the elbow straight and supported on a pillow.
The stroke leg should be brought far enough in front of the body to prevent the patient rolling on to the back, the knee bent and leg supported on a pillow.
A small pillow can then be placed under the patient's waist to maintain the the line of the spine.
When lying on the side position, the patient should have two pillows only under the head.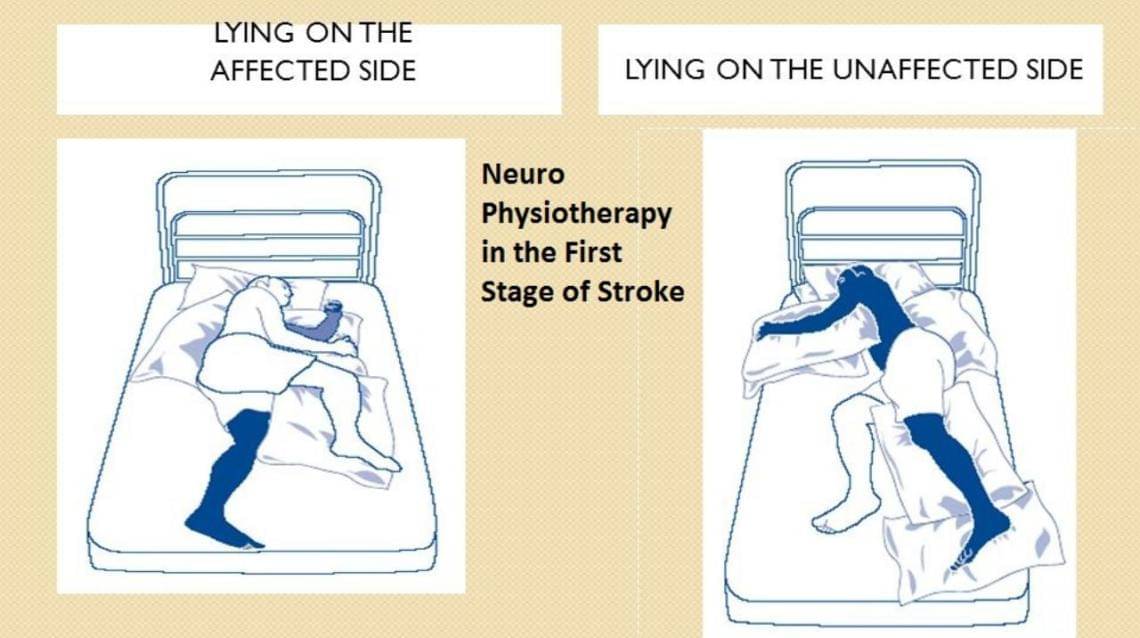
The stroke leg should be brought far enough in front of the body to prevent the patient rolling on to the back, the knee bent and leg supported on a pillow.
A small pillow can then be placed under the patient's waist to maintain the the line of the spine.
When lying on the side position, the patient should have two pillows only under the head.
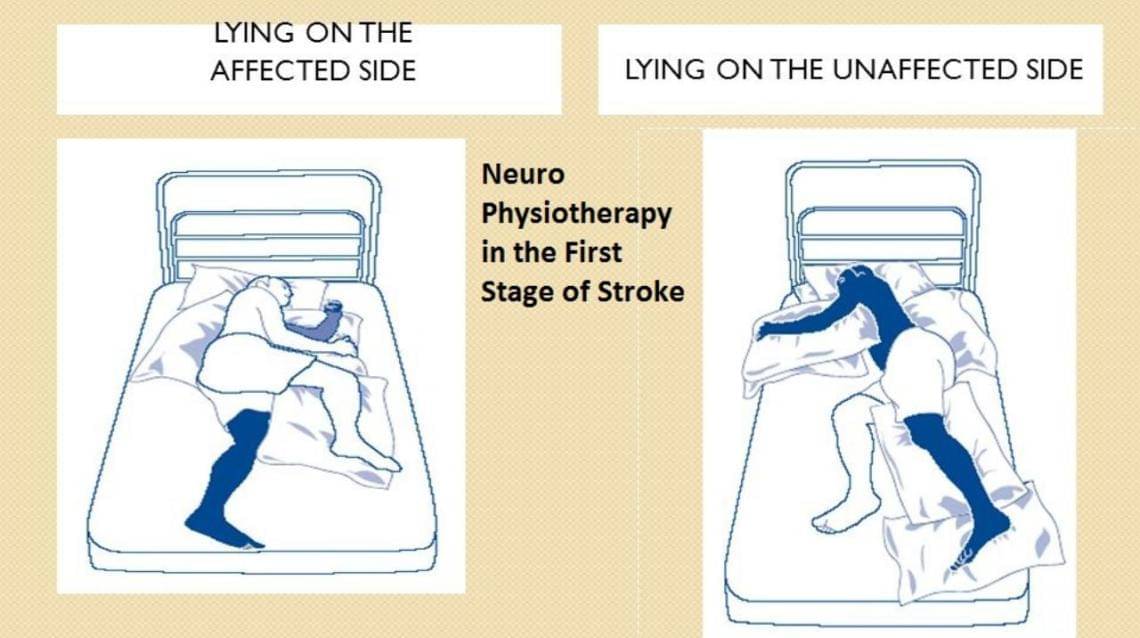
3. Side lying on the affected side:
This should always be encouraged with the stroke shoulder well forward so that the body weight is supported on the flat of the shoulder blade and not on the point of the shoulder.
One or two pillows for head
Place the stroke leg with the thigh so that it is in line with the trunk, and bend the knee slightly.
The unaffected leg should be brought forward and placed with the knee bent on a pillow in front of the affected leg for comfort. This prevents the patient rolling onto his back.
Lastly, bend the head forward a little.
4.Lying supine:
This is the position most likely to encourage spasticity, but some patients do like to lie on their back for a while and it will be required for some treatments.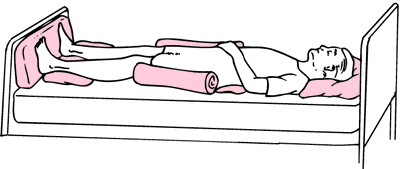
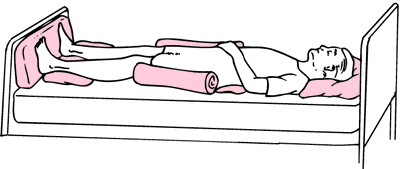
Place two pillows under the patient's head and help him/her bend their head slightly towards their unaffected shoulder and gently turn their head towards their stroke side but do not uses force.
A pillow is placed under the stroke arm which is kept straight at the elbow and if possible, the palms of the hand facing upwards.
The bed must be the correct height to promote independence and safety for the patient, family and health care workers.
5. Sitting up in bed:
Sitting in bed is desirable for short periods only

Must be upright and well supported with pillows
Consider extra support using pillows under arms or knees
Sitting versus lying:
When seated, nearly half of the body weight is supported on 8% of the sitting areas at or near the ischial tuberosities.
Therefore, interface pressures are much higher in sitting than lying
Therefore, interface pressures are much higher in sitting than lying
Distribution of weight when seated normally:
Buttocks & Thighs 75%
Feet flat on floor 19%
Back 4%
Arms 2%
Total 100%
Feet flat on floor 19%
Back 4%
Arms 2%
Total 100%
Pressure relief:
A person who has had a stroke may be susceptible to developing pressure sores
Assess the person and decide on an appropriate cushion use in order to
1.Prevent further skin breakdown,
2.To assist with healing
3.To facilitate the patient to sit out as much as possible