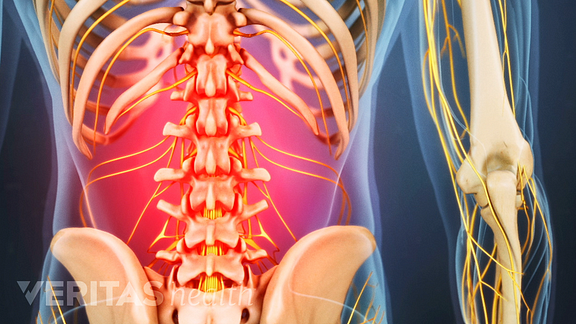
Low back pain (LBP) is a common disorder involving the muscles, nerves, and bones of the back. Pain can vary from a dull constant ache to a sudden sharp feeling. Low back pain may be classified by duration as acute (pain lasting less than 6 weeks), sub-chronic (6 to 12 weeks), or chronic (more than 12 weeks).
Back pain, one of the major musculoskeletal pain problems. Nowadays peoples are mostly affected by this condition, due to our lifestyle changes, loss of physical activity, obesity, eating fast food items, etc..
All of us who treat patients with low back pain have first-hand experience of patients with a long history of chronic pain and disability. Many have had multiple treatments from alternative therapists, physiotherapists, drug therapy, talking therapies, injection therapies and surgery.
Back pain described as “simply a mechanical disturbance of the musculoskeletal structures or function of the back. We cannot diagnose any specific pathology. We cannot even localise the source of most soft tissue pain. Some doctors and therapists do claim to be able to diagnose the site and nature of the lesion in many patients.
Nowadays many more peoples are struggling with LBP. Due to our mechanical life , our working ergonomics, stress and depression, osteoporosis, ageing process etc...
The kind of back pain that follows heavy lifting or exercising too hard is often caused by muscle strain. But sometimes back pain can be related to a disc that bulges or ruptures. If a bulging or ruptured disc presses on the sciatic nerve, pain may run from the buttock down one leg. This is called sciatica.
Kidney pain and back pain can be difficult to distinguish, but kidney pain is usually deeper and higher in the and back located under the ribs while the muscle pain with common back injury tends to be lower in the back. Causes of kidney pain are mainly urinary tract infections and kidney stones
Causes for severe back pain:
Acute low back pain is most often caused by a sudden injury to the muscles and ligaments supporting the back. The pain may be caused by muscle spasms or a strain or tear in the muscles and ligaments. Causes of sudden low back paininclude: Compression fractures to the spine from osteoporosis.
In addition, symptoms of lower back pain are usually described by type of onset and duration:
- Acute pain. This type of pain typically comes on suddenly and lasts for a few days or weeks, and is considered a normal response of the body to injury or tissue damage. The pain gradually subsides as the body heals.
- Subacute low back pain. Lasting between 6 weeks and 3 months, this type of pain is usually mechanical in nature (such as a muscle strain or joint pain) but is prolonged. At this point, a medical workup may be considered, and is advisable if the pain is severe and limits one’s ability to participate in activities of daily living, sleeping, and working.
- Chronic back pain. Usually defined as lower back pain that lasts over 3 months, this type of pain is usually severe, does not respond to initial treatments, and requires a thorough medical workup to determine the exact source of the pain.
Types of Low Back Pain
There are many ways to categorize low back pain – two common types include:
- Mechanical pain. By far the most common cause of lower back pain, mechanical pain (axial pain) is pain primarily from the muscles, ligaments, joints (facet joints, sacroiliac joints), or bones in and around the spine. This type of pain tends to be localized to the lower back, buttocks, and sometimes the top of the legs. It is usually influenced by loading the spine and may feel different based on motion (forward/backward/twisting), activity, standing, sitting, or resting.
- Radicular pain. This type of pain can occur if a spinal nerve root becomes impinged or inflamed. Radicular pain may follow a nerve root pattern or dermatome down into the buttock and/or leg. Its specific sensation is sharp, electric, burning-type pain and can be associated with numbness or weakness . It is typically felt on only one side of the body.
Causes of Chronic Lower Back Pain
Pain is considered chronic once it lasts for more than three months and exceeds the body’s natural healing process. Chronic pain in the low back often involves a disc problem, a joint problem, and/or an irritated nerve root. Common causes include:
Lumbar herniated disc. The jelly-like center of a lumbar disc can break through the tough outer layer and irritate a nearby nerve root. The herniated portion of the disc is full of proteins that cause inflammation when they reach a nerve root, and inflammation as well as nerve compression cause nerve root pain. The disc wall is also richly supplied by nerve fibers, and a tear through the wall can cause severe pain.Degenerative disc disease. At birth, intervertebral discs are full of water and at their healthiest. As people age over time, discs lose hydration and wear down. As the disc loses hydration, it cannot resist forces as well, and transfers force to the disc wall that may develop tears and cause pain or weakening that can lead to a herniation. The disc can also collapse and contribute to stenosis.Facet joint dysfunction. There are two facet joints behind each disc at each motion segment in the lumbar spine. These joints have cartilage between the bones and are surrounded by a capsular ligament, which is richly innervated by nerves. These joints can be painful by themselves, or in conjunction with disc pain.Sacroiliac joint dysfunction. The sacroiliac joint connects the sacrum at the bottom of the spine to each side of the pelvis. It is a strong, low-motion joint that primarily absorbs shock and tension between the upper body and the lower body. The sacroiliac joint can become painful if it becomes inflamed (sacroilitis) or if there is too much or too little motion of the joint.Spinal stenosis. This condition causes pain through narrowing of the spinal canal where the nerve roots are located. The narrowing can be central, forminal, or both, and can be at a single level or multiple levels in the lower back.Spondylolisthesis. This condition occurs when one vertebra slips over the adjacent one. There are 5 types of spondylolisthesis but the most common are secondary to a defect or fracture of the pars (between the facet joints) or mechanical instability of the facet joints (degenerative). The pain can be caused by instability (back) or compression of the nerves (leg).Osteoarthritis. This condition results from wear and tear of the disc and facet joints. It causes pain, inflammation, instability, and stenosis to a variable degree, and can occur at a single level or multiple levels of the lower spine. Spinal osteoarthritis is associated with aging and is slowly progressive. It is also referred to as spondylosis or degenerative joint disease.Deformity. Curvature of the spine can include scoliosis or kyphosis. The deformity may be associated with lower back pain if it leads to the breakdown of the discs, facet joints, sacroiliac joints or stenosis.Trauma. Acute fractures or dislocations of the spine can lead to pain. Lower back pain that develops after a trauma, such as a motor vehicle accident or a fall, should be medically evaluated.Compression fracture. A fracture that occurs in the cylindrical vertebra, in which the bone essentially caves in on itself, can cause sudden pain. This type of fracture is most common due to weak bones, such as from osteoporosis, and is more common in older people.
Common Symptoms of Lower Back Problems
Specifically identifying and describing symptoms can help lead to a more accurate diagnosis and effective treatment plan.
Low back pain is typically characterized by a combination of the following symptoms:
Pain that is worse after waking up and better after moving around. Many who experience low back pain report symptoms that are worse first thing in the morning. After getting up and moving around, however, symptoms are relieved. Pain in the morning is due to stiffness caused by long periods of rest, decreased blood flow with sleep, and possibly the quality of mattress and pillows used.Dull, aching pain. Pain that remains within the low back (axial pain) is usually described as dull and aching rather than burning, stinging, or sharp. This kind of pain can be accompanied by mild or severe muscle spasms, limited mobility, and aches in the hips and pelvis.Pain that travels to the buttocks, legs, and feet. Sometimes low back pain includes a sharp, stinging, tingling or numb sensation that moves down the thighs and into the low legs and feet, also called sciatica. Sciatica is caused by irritation of the sciatic nerve, and is usually only felt on one side of the body.Pain that is worse after prolonged sitting. Sitting puts pressure on the discs, causing low back pain to worsen after sitting for long periods of time. Walking and stretching can alleviate low back pain quickly, but returning to a sitting position may cause symptoms to return.Pain that feels better when changing positions. Depending on the underlying cause of pain, some positions will be more comfortable than others. For example, with spinal stenosis walking normally may be difficult and painful, but leaning forward onto something, such as a shopping cart, may reduce pain. How symptoms change with shifting positions can help identify the source of pain.
Low Back Pain Symptoms by Location
The body’s largest vertebrae are found in the lumbar spine, supporting most of the weight of the upper body. These vertebrae are highly susceptible to degeneration and injury, and an injury at one spinal level can cause a specific set of symptoms:
L3-L4. The L3-L4 nerve root is likely to cause shooting pain in the front of the thigh, possibly including numbness or tingling. Pain or neurological symptoms may radiate to the front of the knee, shin, and foot as well, though it is less common.L4-L5. Pain from the L4-L5 segment typically manifests as sciatic pain in the back of the thigh, and possibly pain that reaches the calves, combined with axial low back pain.L5-S1. Where the base of the spine connects to the sacrum there are a couple of joints that provide support and flexibility. One is the lumbosacral joint, which allows the hips to swing side to side, and the other is the sacroiliac joint, which has limited mobility and mainly absorbs shock from the upper body to the low body.Pain from the L5-S1 segment is generally caused by problems with these joints or from a compressed nerve root. Issues with the L5-S1 segment commonly cause sciatica.
Different nerve roots are irritated depending on the structures in the back that are injured, and being able to point to the specific areas of radicular pain can help more precisely diagnose the source of low back pain.
Symptoms That Require Immediate Attention
Sometimes low back pain can signal a serious underlying medical condition. People who experience any of the following symptoms are advised to seek immediate care.
- Loss of bladder and bowel control
- Recent weight loss not due to lifestyle changes, such as diet and exercise
- Fever and chills
Physical Exam
The goal of a physical exam is to further narrow down possible causes of pain. A typical physical for low back pain includes some combination of the following steps:Palpation. A doctor will feel by hand (also called palpation) along the low back to locate any muscle spasms or tightness, areas of tenderness, or joint abnormalities.Neurologic exam. Diagnosis will likely include a motor exam, which involves manual movement of hip, knee and big toe extension and flexion (movement forward and backward) as well as ankle movement. A sensory exam will likely include testing the patient’s reaction to light touch, a pin prick, or other senses in the lower trunk, buttock and legs.Range of motion test. The patient may be asked to bend or twist in certain positions. These activities are done to look for positions that worsen or recreate pain, and to see if certain movements are limited by discomfort.Reflex test. The patient’s reflexes in the legs will be checked to evaluate weakened reflexes and decreased muscle strength. If reflexes are diminished, a nerve root might not be responding as it should.Leg raise test. The patient is asked to lay on the back and raise one leg as high and as straight as possible. If this leg raise test recreates low back pain, a herniated disc might be suspected.Obtaining an accurate diagnosis that identifies the underlying cause of the pain, and doesn’t just correlate to the symptoms, is important in guiding treatment.Many structures in the low back can cause pain, making the source sometimes difficult to identify.As a foundation of the diagnostic process, the patient provides a detailed description of symptoms and medical history. From this information, a doctor will usually have a general idea of the source of the patient’s paiPatient History
Before starting a physical exam, the patient will be asked to provide information regarding symptoms and medical history. Inquiries typically include:Information about current symptoms. Is the pain better or worse at certain times of day, such as waking up or after work? How far does the pain spread? Are there other symptoms at the same time, such as weakness or numbness? What does the pain feel like—achy, sharp, tight, dull, hot, stinging?Activity level. Does the person lead a generally more active or sedentary lifestyle? For example, does work require sitting at a desk or standing at an assembly line for long periods of time? How often does the person exercise?Sleep habits. As a general rule, how many hours of sleep does the patient get? What sleep position is preferred? What kind of and/or quality of mattress and pillow does the patient use?Posture. What kind of posture feels comfortable or uncomfortable? Does the patient typically sit upright or slouch?Injuries. Has the person had any recent injuries? Has there been an injury in the past that might be relevant now?Answers to these questions provide a doctor with a fuller picture of the patient’s daily life, indicating more specific possibilities for low back pain. A medical history is often the most powerful tool for finding a diagnosis.Physical Exam
The goal of a physical exam is to further narrow down possible causes of pain. A typical physical for low back pain includes some combination of the following steps:Palpation. A doctor will feel by hand (also called palpation) along the low back to locate any muscle spasms or tightness, areas of tenderness, or joint abnormalities.Neurologic exam. Diagnosis will likely include a motor exam, which involves manual movement of hip, knee and big toe extension and flexion (movement forward and backward) as well as ankle movement. A sensory exam will likely include testing the patient’s reaction to light touch, a pin prick, or other senses in the lower trunk, buttock and legs.Range of motion test. The patient may be asked to bend or twist in certain positions. These activities are done to look for positions that worsen or recreate pain, and to see if certain movements are limited by discomfort.Reflex test. The patient’s reflexes in the legs will be checked to evaluate weakened reflexes and decreased muscle strength. If reflexes are diminished, a nerve root might not be responding as it should.Leg raise test. The patient is asked to lay on the back and raise one leg as high and as straight as possible. If this leg raise test recreates low back pain, a herniated disc might be suspected.Usually, a doctor is able to diagnose low back pain based on the information gleaned from a medical history and a physical exam, and further testing is not neededAn imaging scan is sometimes needed to gain more information on the cause of a patient’s pain. An imaging test may be indicated if the patient’s pain is severe, not relieved within two or three months, and does not get better with nonsurgical treatments.Common imaging tests include:X-rays are used to look at the bones of the spine. They show abnormalities, such as arthritis, fractures, Bone spurs, or tumors.A CT scan/Myelogram provides a cross-sectioned image of the spine. In a CT SCAN(Computer Tomography) an x-ray is sent through the spine, which a computer picks up and reformats into a 3D image. This detailed image allows doctors to look closely at the spine from different angles. Sometimes a myelogram is performed in tandem with a CT scan, in which dye is injected around nerve roots to highlight spinal structures, giving the image more clarity.An MRI, or Magnetic Resonance Imaging scan, provides a detailed image of spinal structures without using the radiation required with x-rays. An MRI can detect abnormalities with soft tissues, such as muscles, ligaments, and intervertebral discs. An MRI might also be used to locate misalignments or joint overgrowth in the spine.Injection studies are fluoroscopic-directed injections of local anesthetic and steroid medication into specific anatomic structures. They are helpful in confirming the source of the pain. They are used in diagnosis, in conjunction with rehabilitation, and are considered predictive of surgical outcomes.

No comments:
Post a Comment